Is Achilles pain or stiffness keeping you from living the active lifestyle you deserve?
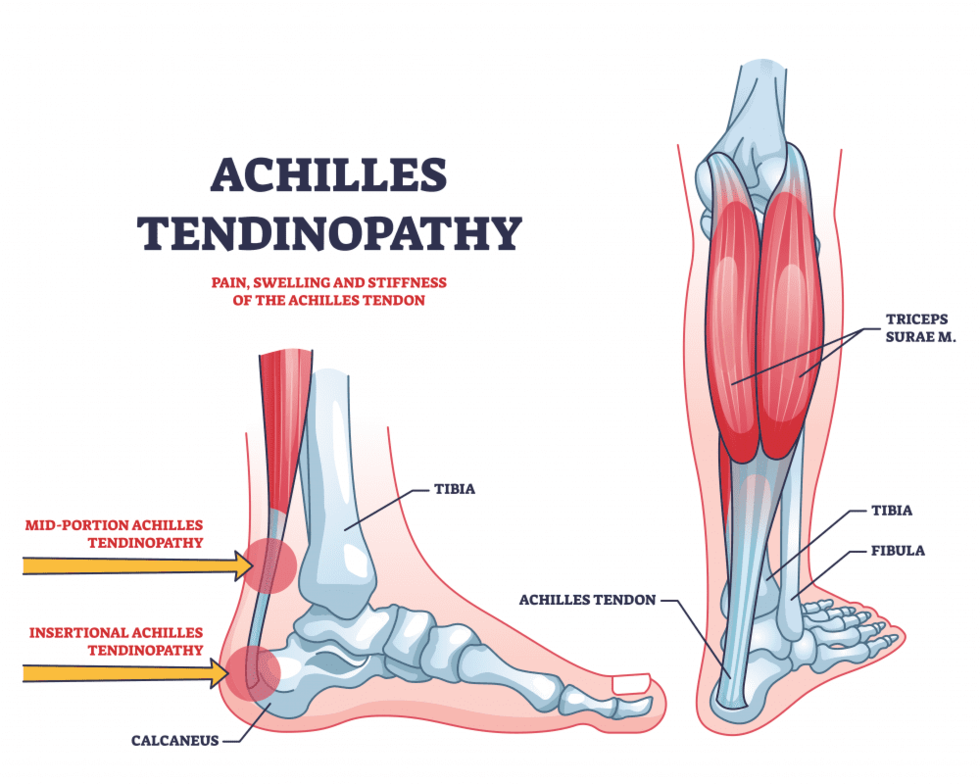
The Achilles tendon is the strongest and largest tendon in the human body. It undergoes high levels of loading during running and jumping related activities with it being responsible for withstanding 6-8x body weight during running.(1) The Achilles tendon connects our calf muscles (specifically the gastrocnemius, soleus and plantaris) to our calcaneus or heel bone. It functions to transfer force from your calf to your foot, to propel you forward during walking, running and jumping related activities. As running speed increases our ground contact time will decrease resulting in increased loading rates to the Achilles tendon.(2) It is thought that these high loads in a repetitive manner can lead to tendon degeneration without sufficient recovery. (1)
It does not only affect runners or active populations though. What was once thought to be an overuse injury, achilles tendinopathy can affect both active and sedentary populations with it being reported only 35% of achilles tendinopathy cases were related to sports in a nationwide registry.(3) Achilles tendinopathy is extremely common in athletes especially in runners with it being reported to affect up to 83% of middle distance runners.(1)
Common symptoms include intermittent pain that may be associated with activity and stiffness with weight bearing especially after prolonged immobility such as sleeping. (3) Pain or stiffness may be present at the start of activity and then improves with time. Common structural changes noted in tendinopathy include increased cross-sectional area, reduced tendon stiffness, and altered viscoelastic properties in both painful and painfree tendons.(1)
In individuals with Achilles tendinopathy we see structural changes leading to a decrease in tendon stiffness. As we age we also see a decline in tendon stiffness. Specifically, a 17% decrease in tendon stiffness has been reported when comparing active 20 year olds to active 70 year olds. (4) While increasing tendon stiffness may sound bad it is actually helpful to improve our ability to transfer force and improve our running economy. A stiffer tendon will transfer force with less elongation or stretch leading to more efficient movement without loss of energy. In contrast a compliant tendon will stretch more under the same load leading to a loss of energy and more muscle work to accomplish the same amount of movement.
To have a full and complete recovery it has been proposed to use a battery of tests that address symptoms, function, structure, and psychological factors. Just because symptoms have resolved does not mean full recovery of function. This may be why Achilles tendinopathy has a high recurrence rate (27-44%) as we want to restore all domains of tendon health. (1)
After a thorough physical therapy examination that may include assessing one’s calf strength, endurance, lower limb motor control, ankle range of motion and joint mobility one can formulate a treatment plan to begin a return to running or sport specific program. If you are struggling to overcome your achilles pain or having difficulties getting back to running or walking please reach out to a qualified healthcare profession like myself.
Below I have laid out a modified protocol presented by Karin Silbernagel and colleagues with some specific consideration for return to running.
Treatment:
Exercise rehabilitation has the highest level of evidence for management of Achilles tendinopathy. (1) Through exercise rehabilitation the goal is to promote remodeling of the tendon, reduce pain, improve plantarflexion endurance, strength and low leg function.(1) Optimal loading has not been established with positive results from isometric, concentric and eccentric protocols.(1) Exercises at higher loads and slow speeds seem to promote tendon strength and size. (1)
Here is an adopted protocol with my own modification for simplicity to follow:
Stage 1: Load management (2 weeks)
During this initial stage the goal is to stop the negative cycle of overloading and injury progression. Complete rest is not indicated as this will lead to tendon underloading which can lead to prolonged recovery. One helpful tool is the pain monitoring model to help clients and clinicians determine how exercise programs should progress or even regress.
Pain Modeling Model:
- Pain scale from 0 to 10; Where 0= No Pain and 10= the worst imaginable pain
- Pain is acceptable to reach 5/10 during and after activity
- Pain the following morning after exercise should not exceed 5/10
- Each week pain and stiffness should not be increasing
During this initial phase we want to progress heel raises up to body weight but may need to start with isometrics, body weight support or aquatic exercises.
- Double leg heel raise on level ground 3 x 10-15
- Single leg heel raise on level ground 3 x 10
- Seated heel raise 3 x 10
- Eccentric heel raise on level ground 3 x 10 (Go up with both feet, lower on one)
- Frequency: 1x/day
Stage 2: Gradual loading (4 weeks)
The goal of this phase is to restore calf muscle strength and improve the load tolerance of the Achilles tendon. To facilitate this progression volume of exercises, range of motion and speed of movement will be implemented during this phase. Heel raises will progress to off a step or use of incline as well as increased speed by performing quick-rebounding heel raises in preparation for plyometrics exercises during the next phase.
- Double leg heel raise on slant board or edge of step 3 x 15
- Single leg heel raise on slant board or edge of step 3 x 10
- Seated heel raise 3 x 10
- Eccentric heel raise on slant board or edge of step 3 x 10
- Quick-rebound double leg heel raise 3 x 20
- Frequency: 1x/day
Stage 3: Restore loading capacity (8 to 12 weeks)
The goal of this phase is to increase external load to transition to heavier strength training and begin running and jumping activities to further promote tendon recovery. Heavier exercises are done 3x/week with lighter body weight heel raise still performed daily (previous phase exercises). To begin running or jumping pain should be very minimal 1-2/10 on NPRS
- Single leg heel raise on slant board or edge of step with weight 3 x 10
- Seated heel raise with weight (preferably machine) 3 x 10
- Eccentric heel raise on slant board or edge of step with weight 3 x 10
- Quick-rebound single leg heel raise 3 x 20
- Plyometric training (including jump rope, hopping, box jump variations)
- Frequency: 3x/wk with rest day in between
It has been proposed that the best prevention is early identification of “minor” symptoms and to adjust loads accordingly during this stage instead of ignoring the symptoms. The earlier symptoms are recognized the shorter expected recovery time if acted upon.
Return to running considerations:
It is recommended to be able to at least hop before initiating a return to run program. Variables to consider when initiating a return to run program include running intensity, frequency, terrain, and shoes. The faster one runs the greater the Achilles tendon demands are so initially adopt a slower pace (don’t let your ego get in the way). Initially, I would recommend having at least one day of recovery between runs and running on the same days you are performing your heavy heel raises (ideally with a 4-6 hour gap between). When considering where to run remember that uphill/incline will increase Achilles demands so try to keep on level ground initially. Also treadmill running has been shown to increase Achilles demands by up to 15% (5). Lastly when considering shoe ware one may elect to adopt a shoe with a higher heel to toe differential to help reduce Achilles demands.
These are just a few of the main variables I would keep in mind when prescribing a return to run program. As one progresses we want to use these to our advantage to fully restore one’s running tolerance.
Just as appropriate loading and exercise is for tendinopathy management it is also essential to note the importance of keeping your entire system in good balance by getting proper sleep, hydration, nutrition and managing stress to help facilitate your recovery.
As always if you have any questions feel free to reach out. If Achilles pain is preventing you from living the active lifestyle you want please don't hesitate for a free phone consulation to see if I am the best option to help!
References:
1)Grävare Silbernagel, K., & Crossley, K. M. (2015). A proposed return-to-sport program for patients with midportion Achilles tendinopathy: rationale and implementation. journal of orthopaedic & sports physical therapy, 45(11), 876-886.
2)Starbuck, Chelsea & Bramah, Christopher & Herrington, Lee & Jones, Richard. (2021). The effect of speed on Achilles tendon forces and patellofemoral joint stresses in high performing endurance runners. Scandinavian Journal of Medicine & Science in Sports. 31. 10.1111/sms.13972.
2)Hughes, Christopher. (2016). Current Concepts of Orthopedic Physical Therapy (4th edition). The Foot and Ankle: Physical Therapy Management Using Current Evidence.
4)Stenroth L, Peltonen J, Cronin NJ, Sipilä S, Finni T. Age-related differences in Achilles tendon properties and triceps surae muscle architecture in vivo. J Appl Physiol (1985). 2012 Nov;113(10):1537-44. doi: 10.1152/japplphysiol.00782.2012. Epub 2012 Oct 4. PMID: 23042907.
5)Willy, Richard & Halsey, Lisa & Hayek, Andrew & Johnson, Holly & Willson, John. (2016). Patellofemoral Joint and Achilles Tendon Loads During Overground and Treadmill Running. Journal of Orthopaedic and Sports Physical Therapy. 46. 10.2519/jospt.2016.6494.





